This article shares information about the common practice of checking for a nuchal cord during the second stage of labour, and unlooping or cutting the cord – interventions that are not evidence-based and can cause birth trauma.
********Updated Jan, 2012:
This article focuses on theories and evidence where routine interventions associated with nuchal cord may be the cause of iatrogenic harm in otherwise-normal birth. This is distinct from cases where umbilical cord entanglement or cord constriction may be the cause of pathological outcomes during gestation, development, progression/descent during labour and birth.
Jen Kamel from VBACFacts eloquently described the risks associated with nuchal cord, which despite studies showing this risk is low will be devastating to the unfortunate 0.4% – 0.6% :
“Even though nuchal cords are common and occur 25% – 35% of the time, rarely a baby’s cord will be wrapped so tightly around their body that the cord is compressed and oxygen delivery to the baby is compromised. When this occurs, a cesarean is prudent and in its absence, a stillbirth could occur. Fortunately, stillbirth from cord accidents, which include nuchal cords and nuchal knots, are rare and occur in 1.5 per 1,000 (0.15%) deliveries. If your baby does have a nuchal cord, the risk of infant death is less than 0.4% – 0.6%. Thus, even though nuchal cords occur in about one third of births, they rarely result in the death of a baby. However, this is no consolation to those who have experienced the horror of their child’s death because when you are the statistic, it doesn’t matter how rarely something occurs.”
********
It is important women are informed about nuchal cord ‘management’ in vaginal birth and how it may affect their baby. Information in this article may assist with birth planning; promote discussion with care providers and birth support; and help to avoid iatrogenic injury.
NUCHAL CORD
A nuchal cord is when the umbilical cord is ‘coiled’ around the baby’s neck. Most nuchal cords are single coils and loose. Less common are tight, double or multiple coils (1,2,3).
Various studies have shown nuchal cord to occur:
- in 10% – 37% of all births;
- more commonly in male babies;
- during pregnancy or labour;
- progressively with longer gestation (1,2,3,4).
Maternity care providers should expect to encounter nuchal cords regularly in their practice (2).

Baby Tyler born with a tight x4 nuchal cord. Babe was pink and breathing spontaneously within a minute, cord intact
NUCHAL CORD RARELY THE CAUSE OF HARM
Nuchal cords are rarely found to be the cause of adverse outcomes in studies of pregnancy and birth. Several authors have concluded nuchal cords “ordinarily do no harm” (5,6,7).
Some studies have associated nuchal cord with an increased rate of variable fetal heart rate decelerations during labour, and tight nuchal cords to a higher proportion of fetal distress and low Apgar scores. (3,4,8) However, in these retrospective studies the definition of tight nuchal cord were those ‘clamped and cut before delivery of the shoulders’ – therefore short-term morbidity was more likely caused by the interventions rather than the presence of nuchal cord (3).
(To learn more about nuchal cords, how babies can and are born with loose/tight/multiple nuchal cords, and why they are disproportionately associated with risk and adverse outcomes, please read Nuchal Cords: the perfect scapegoat.)
RITUAL AND ROUTINE
Many birth practitioners are trained to routinely ‘check’ for a nuchal cord during the second stage of labour, and if present, intervene further by pulling to unloop the cord, or clamping and cutting.
Textbook recommendations to intervene in case of nuchal cords (for normal and emergency births) are based on unevaluated medical literature and lack any references to scientific evidence – they are ‘ritualised’ practices (1).
The rituals advocated in medical textbooks are:
- To conduct a vaginal examination once the baby’s head is born, to feel and check for a nuchal cord.
- To pull and unloop the cord over the baby’s head before ‘delivery’ of the shoulders, if the cord is loose.
- To attempt to loosen the cord or clamp and cut the cord* before ‘delivery’ of the shoulders, if the cord is tight.
* Some textbooks describe the somersault technique as preferable.
While medical literature from the 1840s onward contains cautionary advice about interfering with nuchal cords, ‘revised’ literature since the 1950s does not (1). Influential nursing and midwifery textbooks that teach nuchal cord ‘management’ also fail to include the findings of research and medico-legal reviews that associate risk, serious injury and malpractice with nuchal cord interventions (1).
Practitioners should know routinely checking, unlooping or cutting a nuchal cord is unnecessary and can have serious consequences for the baby. Women and practitioners should be aware these interventions are usually performed without consent and are contrary to the midwifery model of care (1,2,9).
VAGINAL EXAMINATION TO CHECK FOR NUCHAL CORD
A vaginal examination to check for nuchal cord occurs at a vulnerable stage for women, when the baby’s head has just been born. In most cases, women are unprepared for this vaginal exam and have not given informed consent (10,11).
Vaginal exams can be painful and distressing for women, but even more so after birthing the head may have caused pain and possible trauma to the perineum. One woman described her experience to Australian midwife researcher Rachel Reed as “fingers of broken glass digging in” (2).
Checking for a nuchal cord can also interfere with the birth, cause unnecessary stress, and shift a woman’s focus away from giving birth to the intervention being performed (1,2).
No good evidence exists to support the practice of routinely checking for the nuchal cord, yet it is a common medical birth intervention (9). Jefford and colleagues found it is customary practise in US, UK and Australian maternity units, and taught to students in the UK, US, New Zealand, Ireland, Mexico and Canada. (Interestingly, midwives from Norway and Denmark responding to a survey had not witnessed the practice of checking for nuchal cord) (9).
PULLING AND UNLOOPING A NUCHAL CORD
Pulling and looping a nuchal cord over the baby’s head during birth is a common birth intervention (12). Just like checking for nuchal cord, it is not based on evidence and there is growing evidence pulling on the cord may be harmful (4).
For example, evidence indicates that handling the cord stimulates the umbilical arteries to vasoconstrict (reducing blood flow) (13). Pulling on the umbilical cord also creates tension that can risk the cord tearing and “subsequent neonatal bleeding” (6). The effect of pulling on the cord is currently unknown and cannot be predicted– cords have snapped as a direct result this intervention, compromising the baby, mother and practitioner (2).
An Australian study has found that once midwives from USA, Australia, Ireland, New Zealand and the UK felt a nuchal cord, they “reverted to carrying out the intervention they had been taught during their training: to clamp and cut the cord” (2,9).
CLAMPING AND CUTTING A TIGHT NUCHAL CORD
There is no adequate evidence to support routinely cutting a tight nuchal cord (1,2,4,9,14). If the cord is clamped and cut before full delivery has been attempted, on what basis has the practitioner determined the cord was too short or preventing the baby from being born safely? In fact, some of the reasons stated for cutting a tight cord are completely illogical. Surgically clamping and severing the cord does not relieve cord compression or correct a low heart rate/oxygenation – it produces complete, irreversible ligation and amputates the baby from its only source of blood volume, oxygen and oxygen-carrying red blood cells.
As far back as 1842, medical advice about a cord around the neck “so closely as to strangulate the baby”, was to loosen the cord, or if possible “the cord should be left to see if the baby births” – only if the birth is prevented may cutting be required (1). The Handbook of Obstetric Nursing text from 1898 began recommending to feel for a nuchal cord but not to cut if one was found – this advice was continued in midwifery texts until 1930 (1). The 1961 edition of Williams Obstetrics still urged patience after the birth of a baby’s head for the next contractions to ‘deliver’ the shoulders (15). But from 1976 the same book introduced new ideas (without evidence) that if the umbilical cord is tight around the neck, it should be “cut between two clamps and the infant delivered promptly” (15).
When the normal birth process has been “abruptly terminated” a prompt delivery becomes crucial (15, 16). This is not always guaranteed however, and there are number of cases documented in research (Mercer et al) and medical journals where cutting the umbilical cord before delivery of the shoulders resulted in iatrogenic outcomes including cerebral palsy, Erb’s palsy, global developmental delay and death (15).
Although studies show infants may appear to tolerate cutting of a loose nuchal cord, there is clear evidence that cutting of tight nuchal cords before, or immediately after, birth can result in serious injuries and even death (1,14,15). Several writers have observed and documented adverse outcomes as a direct cause of cutting a tight nuchal cord: life-threatening hypovolemia, anemia, shock, hypoxic-ischemic encephalopathy, cerebral palsy (Chow vs Wellesley Hospital 1999) cognitive deficits and death (8,13,14,15,17,18,19,20).
The major risks of cutting a nuchal cord are associated with the effect of compression on the umbilical cord when the coil is tight and the possiblity of a shoulder dystocia (14). Cord constriction from a tight nuchal cord can produce a loss of blood volume in the baby and cause acid-base imbalance (due to arteries continuing to send blood away from the baby, but impeding venous return) (14). With cutting of the cord, the baby’s low blood is “fixed” with no recourse to placental transfusion to correct this dangerous condition (14). (Placental transfusion is part of the normal birth process that can reperfuse the baby with oxygenated blood once the baby has been born and compression on the cord is relieved (14)). In serious cases of late-stage cord compression/ tight nuchal cord, babies can be born exhibiting “pallor, irregular respirations, low Apgar scores, gasping, tachycardia, weak peripheral pulses, hypotension, and acidemia” (21). With the cord already severed, these babies are unable to receive placental transfusion and correction of these conditions.
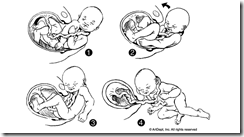
In 1991, the somersault manoeuvre was first described as an option for ‘managing’ a tight nuchal cord without cutting (6). Although not an evidence-based practice, the somersault manoeuvre preserves the normal anatomy and physiological processes of birth by keeping the cord intact – which is necessary for placental transfusion during the third stage of labour/ neonatal transition and vitally important for the baby born deplete in blood volume (14).
CONCLUSION
Routine checking and intervening with nuchal cords, without evidence it is beneficial or required, is in stark contrast to the philosophy of evidence-based practice – and particularly the midwifery model of care of non-intervention in normal physiological birth.
Practitioners that respond clinically, not routinely, to a nuchal cord – and with the least intervention possible – are more likely to protect normal physiology and anatomy and avoid iatrogenic injury.
When practitioners begin to observe babies being born with a nuchal cord without intervention, they will also cease to routinely check for nuchal cord – thus sparing women the indignity, pain and distraction of a vaginal exam as their baby is being born.
Until nuchal cord ‘management’ ceases to be routine practice, women are best advised to discuss these interventions with their care providers. Women can insist upon interventions being performed only when required and where supported by evidence. Birth partners and doulas should also be aware of nuchal cord rituals and have a clear understanding of the woman’s preferences for the second and third stages of her labour.
Further reading
BIRTH STORIES
An Australian mother’s experiences of her baby’s tight, double nuchal cord being cut before birth (hospital)
An American mother’s similar experience (hospital birth)
A mother shares a birth story of her baby’s nuchal cord cut before birth and requiring specialised care
Compare these experiences with this homebirth of a baby born in the caul with x4 times nuchal cord
Umbilical cord around baby’s neck rarely causes complications – VBACfacts website – excellent article with concise summary of research evidence, as well as various heartfelt comments from parents of babies that experienced benign nuchal cords, harm from pre-birth or immediate cord cutting, harm from delay in intervention despite evidence of fetal distress, fetal loss and stillbirth.
Read Nuchal Cord Management and Nurse-Midwifery Practice (pdf)
REFERENCES
(1) Jefford E., Fahy K., Sundin D. (2009) Routine vaginal examination to check for a nuchal cord Br J Midwifery, 17(4)
(2) Reed R. (2007) Nuchal Cords: Think Before You Check, The practising midwife, 10(5), 18, 20.
(3) Lt Col G Singh, Maj K Sidhu (2008)‘Nuchal Cord: A Retrospective Analysis’, MJAFI, Vol. 64, No. 3
(4) Reed, R. Barnes, M. and Allan, J. (2009), ‘Nuchal cords: sharing the evidence with parents’, British Journal of Midwifery, February 2009, Vol 17 (2): 106-109.
(5) Cunningham FG., Leveuo J., Bloom SL., Hauth JC., Gilstrapp III LC.,Wenstrom KD. (2005) Williams Obstetrics 22nd edn. McCraw-Hill Medical Publishing Division
(6) Schorn M., Blanco J. (1991) Management of the nuchal cord. J Nurse Midwifery ;36:131–2.
(7) Steinfield J., Ludmir J., Eife S., Robbins D., Samuels P. (1992) Prenatal detection and management of quadruple nuchal cord: A case report. Journal of Reproductive Medicine 37(12): 989–91
(8) Cashmore J. Usher RH. (1973) Hypovolemia resulting from a tight nuchal cord at birth. Pediatr. Res: 7:339.
(9) Jefford E., Fahy K., Sundin D. (2009) The Nuchal Cord at Birth: What Do Midwives Think and Do? Midwifery Today 89: 44–6
(10) Coldicott Y., Pope C., Roberts C. (2003) The ethics of intimate examinations -teaching tomorrow’s doctors. BMJ 326(7380): 97–101
(11) Lewin D., Fearon B., Hemmings V., Johnson G. (2005) Women’s experiences of vaginal examinations in labour. Midwifery 21: 267–77
(12) Jackson H., Melvin C., Downe S. (2007) Midwives and the fetal nuchal cord: asurvey of practices and perceptions. J Midwifery Womens Health 52(1): 49–55
(13) Coad J. & Dunstall D. (2001). Anatomy and Physiology for Midwives, Mosby.
(14) Mercer J., Skovgaard R., Peareara-Eaves J., Bowman, T. (2005) ‘Nuchal Cord Management and Nurse-Midwifery Practice’, Journal of Midwifery & Women’s Health 4 (23): 373-79
(15) Iffy L., Varadi V. and Papp E. (2001). ‘Untoward neonatal sequelae deriving from cutting of the umbilical cord before delivery’. Med Law, 20 (4): 627-624.
(16) Wickham S., (2008) Midwifery: Best Practice Vol 5. London, UK
(17) Dhar K., Ray S., Dhall G. (1995) Significance of nuchal cord. J Indian Med Assoc;93:451–3.
(18) Shepherd A., Richardson C., Brown J. (1985) Nuchal cord as a cause of neonatal anemia. Am J Dis Child;139:71–3.
(19) Iffy L., Varadi V. (1994) Cerebral palsy following cutting of the nuchal cord before delivery. Med Law;13:323–30.
(20) Flamm M D. (1999). ‘Tight nuchal cord and shoulder dystocia: a potentially catastrophic combination’. The American College of Obstetricians and Gynecologists, 94 (5): 853.
(21) Vanhaesebrouck P., Vanneste K., De Praeter C., Van Trappen Y., Thiery M. (1987) ‘Tight nuchal cord and neonatal hypovolaemic shock’, Archives of Disease in Childhood, , 62 1276-77
Additional articles
Jackson H., Melvin C., Downe S. (2007) ‘Midwives and the fetal nuchal cord: a survey of practices and perceptions’. Journal of Midwifery and Womens Health 52: 49-55
Janet D., Larson MD., William F., Rayburn MD., Crosby RSS., Gary R., Thurnan MD. (1995) Multiple cord entanglement and intrapartum complications. Am J Obstect Gynecol 173:1228-31.
Nelson K., Grether J. (1998) Potentially asphyxiating conditions and spastic cerebral palsy in infants of normal birth weight. Am J Obstet Gynecol 1998;179:507–13
Melvin C., Downe S. (2007) Management of the nuchal cord: a summary of the evidence, Br J Midwifery 15(10) 617-21
Walsh, D., Downe, S. (2010) Evidence for Neonatal Transition and the First Hour of Life, Essential Midwifery Practice: Intrapartum Care pp. 85-89.



Some years back some of my collegues became interested in the physiology and management of the nuchal cord.They did an extensive literature revue . As a result of this we have been somersaulting babies out for quite some time.The apgars are better and the whole atmosphere is less fraught.
Posted by Jacinta Hay | November 5, 2011, 12:52 amThanks Jacinta – great to hear the practice has modernised where you work.
I’ve read elsewhere responses to this article where some practitioners are skeptical of hesitating to routinely cut a nuchal cord, but even a cursory review of the literature should make them reconsider. No practitioner should face sticky shoulders or a dystocia after the cord has already been cut, the results can be catastrophic.
Posted by GiftedBirth | November 5, 2011, 3:13 pmI have been using this procedure also and cannot believe how easy and effective it is. Should be taught to all practitioners.
Posted by Caroline Walker | January 15, 2013, 7:32 pmI have to say this is the best well researched article I have seen in a while on nuchal cords! I teach childbirth classes and needed something like this to share with my students. Thank you!
Posted by Stacy Lewis (@avocadobaby2) | November 5, 2011, 3:54 amYou’re welcome Stacy, all the best with the CBE!
Posted by GiftedBirth | November 5, 2011, 3:05 pmAn excellent article, and one I am sharing…thank you so much for a great article, and more support for an evidenced based practice! I have only attended about 80 births so far, but have never cut a cord on the perineum. I try to wait til it’s limp and white, even if the baby has had sticky shoulders, or needed to be born quickly. I want to let the baby get all it’s blood, and 30% of it is in the cord and placenta. Thanks again! Cathi Cogle, CPM
Posted by Cathi Cogle | November 5, 2011, 5:17 amCathi, thank you for your response and assistance with editing. It was one thing I asked for when posting to the CordClamping facebook page – help with proofreading.
Great to hear about the babies experiencing a physiological transition rather than pathological.
Posted by GiftedBirth | November 5, 2011, 3:04 pmI am a danish midwife and have delivered a lot of babies during my 8 years of practice. I have learned to check the cord very carefully, but from mothers front (and not near the perineum). Loosen gently, but only cut in extreme cases. I never had to cut a cord before delivery – and I think this practice is most common in Denmark. I think most midwifes or doctors never have tried it or rarely.
Best regards
Posted by Anne Mette | November 9, 2011, 6:55 amI’ve had six babies and never had a cord around the baby’s neck. I’m undecided if I would want to forgo a check for this or not. It seems to me that once a baby’s head is born, the body follows so quickly that there may not be much time to even check for the cord.Perhaps if there is a delay of the baby’s body being born, in conjunction with heart deceleration, then the nuchal, could be the cause. But I do agree that intervention should be the result of evidence.
Posted by Sherry | December 4, 2011, 3:53 pmWhat do you suggest for babies that aren’t breathing? My LO was born blue with a tight cord and needed to be resuscitated. Later he had seizures and it was found that he had brain damage from the oxygen deprivation.
Posted by Olivia ♡ | December 8, 2011, 7:41 pmHi Olivia,
Thank you for your message. I’m very sorry your son suffered HIE from a placental abruption and oxygen deprivation at birth. Your website and everything you do for your son is truly amazing.
Regarding your question about what to do when a baby isn’t breathing?
In birth without complications, babies can be a blue/purple colour while placental circulation persists. Where a tight cord may have temporarily reduced a baby’s blood volume, initial respiration may be delayed until the baby’s blood volume has been restored and the lungs perfused (by oxygentated blood transfusing from placenta back to the baby).
It is very common in a hospital setting for babies to have immediate cord clamping in order to relocate for resuscitation (this is standard protocol in most cases still). However, researchers that specialise in fetal to neonatal transition argue this cuts the baby from any chance of having low blood volume, poor oxygen levels and acidosis corrected via placental transfusion. Some practitioners now urge that resuscitative measures/protocol include an intact umbilical cord. The B.A.S.I.C.S trolley was designed for hospital staff to bring the resuscitation equipment to the baby, instead of vice versa (where the placenta and umbilical cord are still functioning and there is benefit from keeping baby attached to placenta with cord intact).
You may be interested in referring to the Links section to access the research papers on nuchal cord management.
This article and the above information really only relates to the presence of a nuchal cord tight enough to cause complications (cord compression, decels during labour, reduced blood volume) in the absence of other complications, such as placental abruption.
Wishing you and your family all the best Olivia
Posted by GiftedBirth | December 8, 2011, 11:47 pmI use the summersault method to deliver infants with nuchal cords and teach it to the residents and PAs that I work with. But some years ago I knew of a MD that attended a woman that presented with no care with infant starting to crown. After the head delivered he noted a cord and cut it and delivered the body. Much to his suprise he noted the the infants umbilical cord was intact. Yes she was pregnant with twins and he cut the cord of the 2nd baby. He had to go in and do a breach extraction!!!
Posted by Sally Prickett | December 15, 2011, 11:28 amThis article and your response to Olivia regarding her son’s birth has prompted some further questions for me. My first born son was born still in January 2011 after a “textbook” normal physiological delivery at term. His heart was monitored throughout the final hours of labour, and he showed no signs of distress. We have a clear reading of his heart 3 minutes before his delivery. He did not have the cord around his neck, and there were no other complications such as placenta abruption. Postmortem results showed he was perfectly formed with no heart or lung defects, there was no meconium in his airways or lungs, he had no hypoxic brain changes and no one can explain what happened. The moment he was born he was totally limp, and scored 0 on the agpar scale, so although he was handed to me for 2 seconds still attached to the cord, the medical team reacted to his still body, grabbed him back, clamped and cut the cord and placed him on the resus. trolley for immediate intervention. They tried to get him to breath for an our and a half, CPR, adrenaline, etc. whilst giving him oxygen, totally confused as to why he was not breathing and would not respond. Babies are resilient I am told, especially 8lb 1oz babies with no heart defects, so the questions remain unanswered. I am now wondering if his cord had not been clamped would he have had a chance of survival through placental transfusion? Apparently my placenta was also healthy and showed no signs of degradation. I am now pregnant again, and considering birthing options so answers to these questions would provide me with some much needed insight and respite. Many thanks.
Posted by Sofia | March 14, 2012, 10:45 pmDear Sofia
I am so very sorry you lost your precious baby boy at birth…what a tragic loss for you and your family. It must be a heavy burden to have these questions and the cause of his death unanswered as you carry new life inside you. I will write to you privately to discuss your birth experience and your birthing options for your unborn baby.
In brief, delayed cord clamping may offer some physiological as well as psychological benefits to you and your baby at your next birth. The mother and baby contact may assist with maximising your hormonal response at birth and may help to avoid any distressing triggers (such as separation, observing your baby being handled away from you etc).
Regardless of your birth choices Sofia, I am also aware that some mothers that have experienced a previous stillbirth or loss have found the emotional support (during pregnancy and birth) by a doula or independent midwife to be invaluable.
Please check your email for a message from me in the next day or so.
Much love.
Kate
Posted by GiftedBirth | March 16, 2012, 11:39 pmLotus Birth provides the optimum situation for babies and mothers. it greatly reduces the trauma of C/section.
http://www.lotusbirth.net
Posted by Rachana Shivam | June 8, 2012, 11:57 pmReblogged this on mumanu pregnancy pillow and commented:
I really love this article. I have a lot of clients who have had caesareans for failure to progress and discovered that baby had the cord around their neck. The woman is totally relieved that the caesarean ‘saved’ her baby. However, “Nuchal cords are rarely found to be the cause of adverse outcomes in studies of pregnancy and birth. Several authors have concluded nuchal cords “ordinarily do no harm” “
Posted by Mumanu | November 22, 2012, 7:18 am27 years ago, my son was delivered vaginally, I was in a kneeling position, and he delivered with the cord wrapped around his neck. My husband tells me my son was not breathing. I did not see my son for several hours and I had to ask to see him. The whites of his eyes had brown dots from the delivery. I and my son were checked on frequently by the mid-wife that evening. My.
son had OCD symptoms at an early age, first his socks, his underwear, his hands, scrubbing his face raw, issues with sleeping and bedwetting till 13 years. He would throw fits. Never happy. His perception of his school day was always different from his sister’s. She’d tell me she saw him happily playing and he would tell me the opposite. Then he started playing sports and getting injured. He had a very jarring off road motorcycle accident that broke both bones in both legs. He had another accident that split his helmet and yet another where he suffered at least a 2 1/2 minute seizure. He was like a rage doll at times because meds did not agree with him. He ended up with high anxiety and extreme anxiety horrors from age 16 due in part to hormones, risk taking behavior (depression). He slept for basically 2 years except when tutors came home. He was under the 504 program at school but was not allowed to march with his class. The horrors are better now for periods of time and then he gets in trouble with the law. I have always felt the cord strangulation started our path and if I had known more..My son is bright but has not found his path in life because the other issues keep him down.
Posted by Linda Cyr | November 22, 2012, 3:15 pmLinda, I’m very sorry for your son’s anguish and how challenging and painful it must sometimes be as his mother.
You mentioned that your son was born with a nuchal cord and that you then didn’t see him for several hours? This blog post is specifically focused on the effect of intervention during, and immediately after birth. In particular, the impact of amputating the baby from the placenta before the baby has the chance to redistribute the “lost” blood volume, due to cord compression, back to the baby.
I sincerely hope my article does not create anguish for those where the presence of a nuchal cord was the source of injury or complication during labour or birth.
Wishing you and your son all the best,
Kate
Posted by Kate Emerson | November 23, 2012, 1:17 pmNever stop praying for him and your family God is an all time healer with many blessing your family is in my prayers
Posted by Adriane Butler | December 14, 2012, 2:31 pmI find this really interesting. My 7.5 yo was born with a nuchal cord. His father remembers not being able to cut the cord as planned because of this. He believes they cut he cord from our son after he was completely delivered. My son has been diagnosed with Global Developmental Delay. He is not on the autism spectrum but has a lot of autistic tendencies. As he gets older, I always wonder if he was deprived of any (or enough) oxygen to his brain due to the nochal cord to have contributed, at least in part, to his diagnosis. Since a lack of oxygen can affect the brain and stem cord, it’s hard not to think it had some part.
Posted by Shannon F | December 16, 2012, 3:57 pmWhat a brilliant article! I just wrote a piece on the topic of early cord clamping, but a sharp reader linked this page for additional – and very valuable – information. I have added a note to the end of my article and recommended that people read this. Wish I’d been aware of Delayed Cord Clamping before completing mine, as it would have been better.
Posted by Heidi Stevenson | December 2, 2012, 8:26 amnow what happen, FB. my cousin is Diaz s wife her daugther Jhundelisse Diaz born April 1, 2013, was wrapping her neck with cord first time and stay hospitlal IUC. put breathing tube her nose…. This is baby s life..hope is well soon go home next week friday..i pray.. that is normal…
Posted by Isabel Diaz | April 6, 2013, 10:45 amReblogged this on Birthing Change and commented:
Bringing some birth back to Birthing Change, here is an interesting article about nuchal cords (umbilical cord around baby’s neck).
Posted by Birthing Change | September 24, 2013, 10:49 amReblogged this on Maggie Marie and commented:
What you should know abut the baby’s cord and clamping…
Posted by lovemags | September 25, 2013, 3:28 amA very informative article. I have experienced a stillbirth of my DD at 35weeks due to a true tight knot. I did not experience any reduced fetal activity during the last days, but just a few hours before the baby stopped moving she was moving continuously, which I assumed then to be normal movement. But after that she totally stopped moving and when we went to the doc there was no heartbeat. After delivery it was noted that she has a true tight knot which caused this. The doc had mentioned that it could have been a knot that was tightened when the baby moved head down. Now I am at 32 weeks and this time during my 32 week scan doc observed a single loop around the baby’s neck. I am totally scared if that will compress the chord or come out of the neck and form another chort knot. I just wanted to know if such a thing is possible and also if the Wharton’s jelly will prevent compression of the chord then why does true tights knots and Chord compressions occur.
Posted by Anne Thomas | May 12, 2015, 8:30 pmI am a paramedic instructor (and a paramedic obviously), and stumbled across the article in preparation of some training.
So, understanding that we (paramedics) are not OB specialist, and that most of the OB calls we get are a minority and under difficult circumstances…that we are often put into that position without warning and with a very high expectation of performance, and that we are genuinely trying to help. We do not have the option of “waiting” for “expert help”. We are expected, compelled to act when requested. In that context, I have the following questions:
1) Can you explain why it is less harmful to cut a loose nuchal cord than a tight one. It seems that the opposite would be true with cord compression already taking place.
2) The advise you give above (if I read it correctly) is not cutting a cord unless progression of the baby is impeded.. What clinical signs do you look for that can help us tell the difference when that occurs? I am not trying to be crude, but it’s all a bloody mess under low light conditions and cramped quarters when we are involved, not a birthing center.
3) You have talked about when NOT to cut the cord, but how about when to actually do it? Understanding that it is not common practice in the US for paramedics to “check” for nuchal cord, when we see one it is after delivery of the head (or a loop protruding during breech). Other than checking for “pulsation” (how effective is that anyway?) What simple advice do you have for when to cut the cord, other than when not to?
And a final comment to the midwives out there (here is where I piss you guys off) : We in EMS are indeed here to help and we want to help. So I ask that you understand that we as paramedics do not go into these situations looking to “oppress women” or “impede the birthing process”…all of which we have been accused of when responding to birthing centers (which we only do when someone requests us). Unfortunately our culture is one of “doing” and “acting”, not waiting. This is where our cultures clash. it has nothing to do with an anti-woman agenda. Please understand that.
In addition, I have never seen a birthing center with a well defined, practiced, rehearsed emergency action plan for when 911 gets called or what happens after we arrive. From our side of the fence, it seems that “midwives do the midwife thing” until something goes horribly wrong, call 911 at the last minute, and then get very upset when we show up and do “the paramedic thing”. 90% of the issues could be avoided with pre-planning and dry runs that respect each others goals and methods. In that area, the birthing centers I have had contact with fall far short. I don’t doubt your expertise, just your willingness to work with EMS and do pre-planning. Given the high stakes, thats an area we both should work on.
Posted by croaker260 | October 7, 2015, 8:19 amThank you for your comment – am I correct in thinking you’re from the US? I really like your suggestion of emergency drills and simulation training for birth centre staff with EMS. I’m Australian and do not have adequate knowledge of the different tiers of training in the US to comment further on this. In Australia all midwives are university/clinically trained.
To answer Q 1) Cutting a tight cord is harmful, because strong tension on the cord (combined with normal temporary compression on the cord) during second stage can impede blood flow via the umbilical vein (thin walled vessel). The blood flow in the arteries is under higher pressure from the fetal heart, so blood to the placenta may continue while restriction on the vein can impede blood returning back to the baby. This can result in loss of volume within the fetus/neonate. Cutting a tight nuchal cord risks severing the baby from their blood supply at a time where they could be fatally hypovolemic. An intact cord at the time of birth allows for release of tension on cord, restoration of blood volume back to the baby, perfusion of the lungs and adequate cerebroperfusion/ oxygenation to restore consciousness (if baby is compromised by temporary inadequate perfusion/oxygenation during second stage labour).
Q2) I have discussed nuchal cord management with many clinically trained midwives, and of those that practice intact cord at birth – they have never had a cord actually impede a birth. If the shoulders have turned and delivered, but the cord is tight and baby isn’t budging after the shoulders, then somersaulting the baby’s body out instead of pulling away from the mother is the appropriate response to prevent additional tension on cord/ cord avulsion.
Q3) I feel unsure answering this question, because there are no absolutes in childbirth. Eg. An OB aware of feto-maternal hemorrhage may clamp the cord as soon as possible to prevent blood loss and prepare the baby for transfusion. Damage to the cord and placenta may similarly necessitate clamping the cord to prevent neonatal blood loss. In a normal birth, the cord should not be touched until after transition to pulmonary respiration is complete and the fetoplacental circulation has ceased. The cord will be thin, white and floppy. This may take 5mins to 15mins (sometimes more). An intact cord provides access to warm, whole blood for a baby during resuscitation, that may be temporarily hypovolemic at the time of birth. Simple advice for cutting the cord, where mother-baby does not require separation is only when the mother asks. Where separation is necessary (for urgent medical assessment/treatment), the cord should not be clamped prior to the baby establishing regular respirations where ever possible. For resuscitation, the cord can remain intact for intial assessment, stimulation, bag & mask etc – and may only need clamping and cutting to relocate baby if initial assessment/attempts have identified the need to commence more invasive measures. Keeping cord intact is compatible with the first steps of standardised resuscitation guidelines, and the perfusion of 30-60s of delayed clamping may actually prevent the need for more invasive measures if the infant was only mildly compromised.
Thanks again for your comment. You may enjoy reviewing the recent literature on bedside resuscitation for more information about intact cord care and maternal experience of neonatal resuscitation next to their baby.
Thank you for your care and expertise in emergency services 🙂
Posted by Kate Emerson | October 9, 2015, 11:56 am